Start a healthier life now with the carnivore diet!
Your wellness objectives are within reach with the support of our community and coaches.

HOW IT WORKS
You set your objectives.
We'll support you.

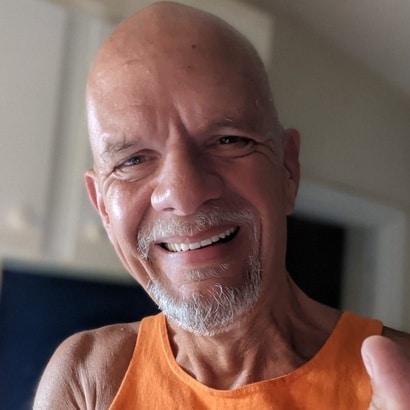
Carnivore diet guides
Step-by-step video guides by Dr. Shawn Baker.

Join the community
Meet Dr. Shawn Baker and other members!

Meal plan & recipes
Trust the process in the world’s simplest diet.
IS IT FOR ME?
You are worthy
of better health.

Enjoy a diet without hunger or cravings
Gone will be the days when you’re hangry if you don’t snack. You very well may experience true satiety for the first time in a long time, perhaps ever. You will probably not want to go back!
Get Support On Your Journey
Our community, coaches, and Dr. Baker are here to guide you through the journey we all have been through. Lean on the community during your adaptation and afterwards! It only gets better!




Claim your health back
Achieving your ideal weight is just one part of the journey. It is a bonus to getting healthier on the carnivore diet.
Meet our coaches
Our coaches complete a certification program prepared by Dr. Shawn Baker and provide personal coaching as well as group coaching in our community meetings throughout the week.
Personal approach. Sustained results.
You set the pace and we’ll support your journey to the results you desire. We are here for you and you will feel supported in your choices.
WHAT TO EXPECT
Community at your fingertips

Find the foods you crave and enjoy
Refer to our recipes, meal plans, or shopping lists! Get tips from our coaches on how to prepare easy meals or eat out. Whatever your situation, we’ll help you figure out what will work best for you!

Knowledge up
Browse through the research articles in our library, read up on carnivore diet facts, tips, and tricks, and get helpful advice about adapting your lifestyle. Our articles, guides, and podcast episodes have it all.

Get the support you need
Community is where it’s at. Our members and experts are here to support you along your journey. Get the support you need and become an inspiration to others after you.
800+ SUCCESS STORIES
Real people, real results.